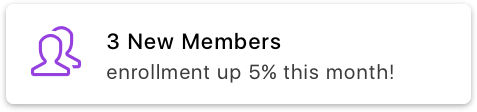
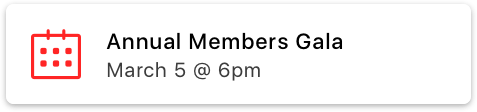
SilkStart's software simplifies membership and association management. Connect with your members like never before.
Easy
Manage and grow your member-based organization in the cloud
Modern
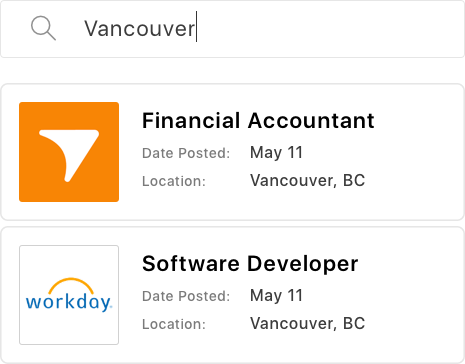
Delight your members with a simple interface that works on any device
Flexible
No two organizations are the same - your platform is tailored to your needs.